33F with fever and body pains since 5 days
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
A 33 year old female a homemaker belonging to middle class according to modified kuppuswamy scale presented to general medicine OPD with C/o
Fever since 5 days along with dry cough, cold, headache and body pains
Burning micturition while using medicine
HOPI
Patient was apparently asymptomatic 5 days back then she had fever which was intermittent in onset, high grade associated with severe body pains, dry cough, cold and headache along with retro orbital pain since 5 days with no aggravating factors and temporarily relieves on medication.
Also complaints of burning micturition while taking medicine
No vomitings and diarrhea
Past History
N/K/C/o diabetes,hypertension,TB,asthma,epilepsy
No previous surgeries
Menstrual History
Attained Menarche at 12 years
Has regular cycles 5/28
Moderate flow
Not associated with clots and pain
Family History
Not significant
Personal History
Mixed diet
Appetite - normal
Regular bowel and bladder movements
Burning micturition while taking medication
Sleep - adequate
No known allergies and addictions
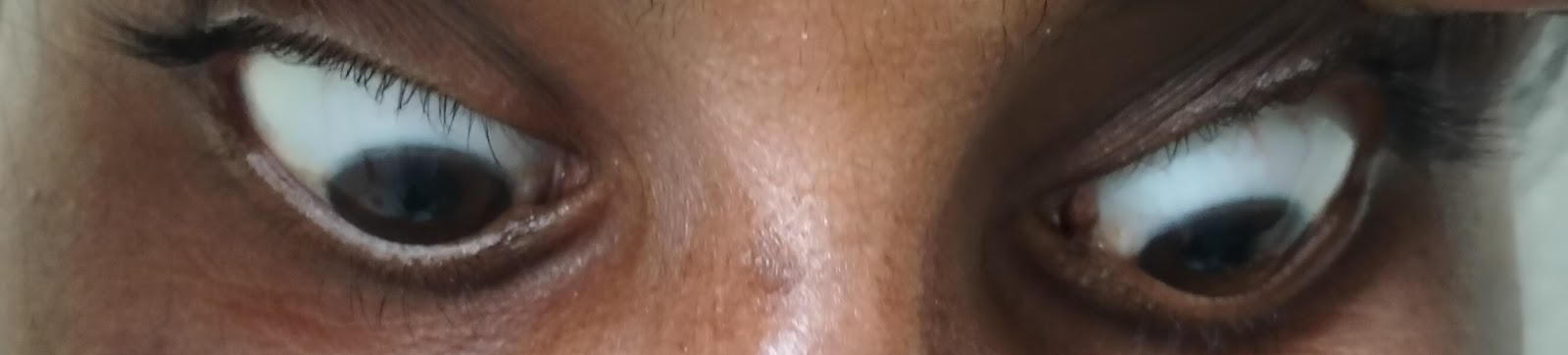
GENERAL EXAMINATION
Patient was C/C/C
Moderately built and nourished
Weight- 52kgs
No signs of pallor,icterus,cyanosis, clubbing,pedal edema and lymphadenopathy
Vitals
Temp - 100.5F
BP - 90/60mmHg
Pulse rate - 70bpm
RR - 20 breaths/min
Systemic Examination
CVS - S1,S2 heard,no murmurs
RS - normal vesicular breath sounds heard
CNS - No neurological deficits
Per abdomen - soft and non tender
Provisional diagnosis
Viral pyrexia
Treatment
Paracetamol 650mg every 6th hourly
4th hourly temp check
11/10 - evening - 101.3F
11/10 - night - around 100F
12/10 morning 102.1F




Comments
Post a Comment