63M came with c/o fever,cough,difficulty in breathing
Hi!! This is Vijaya ratna,9th semester medical student.This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
A 63yr old male patient came with the complaints of fever,cough since 1 month and difficulty in breathing since 2 days
HOPI
Patient was apparently asymptomatic 1 month back and then had fever intermittent in onset, low grade, associated with chills and rigors,no diurnal variations,no aggravating factors relieved on medication
C/o cough since one month associated with sputum sometimes
C/o difficulty in breathing since 2 days
PAST HISTORY
K/C/O CAD Post PTCA status 8 yrs back
K/C/O HTN since 3 months but not on any medication
H/o blood transfusion 8 days back - 1 PRBC ,
N/K/C/O DM , CVA , Asthma , TB, Epilepsy
PERSONAL HISTORY
Diet : mixed
Appetite: normal
Sleep : adequate
Bowel and bladder : regular
Addictions:
Alcohol - used to consume alcohol stopped 15 yrs back
H/o smoking + but stopped 15 yrs back
FAMILY HISTORY
Not significant
GENERAL EXAMINATION
Patient is conscious,coherent and cooperative
He is Ill built and malnourished
VITALS
Temperature - 101 F @4pm
100 F @5pm
98.7 @6pm
BP
PR - 96bpm
RR - 16cpm
SYSTEMIC EXAMINATION
CVS - S1 S2 heard,no murmurs
RS - BAE PRESENT NVBS HEARD
P/A -Soft , non tender
CNS -NFND
21/10/23
PROVISIONAL DIAGNOSIS
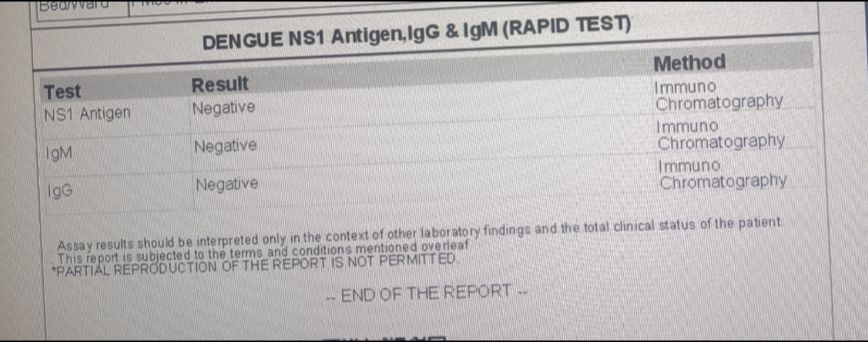
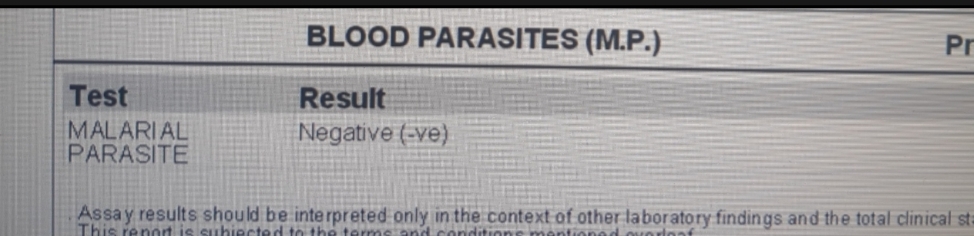
PYREXIA UNDER EVALUATION , HEART FAILURE (EF - 54%) SECONDARY TO CAD - S/P PTCA 8yrs back
TREATMENT
IV fluids : UO + 30ml/hr
Inj.NORADRENALINE (6ml/hr IV infusion ) increase /decrease according to BP - 0.16mg = 1 ml
Tab. ROVASTATIN + CLOPIDOGREL PO/HS (75MG + 10 MG )











Comments
Post a Comment