A 60 YEAR OLD MALE WITH LOSS OF APPETITE AND PEDAL EDEMA
VIJAYA RATNA DANDE 34
Hi,I am Vijaya ratna 3rd sem Medical student.This is an online elog book to discuss our patient's health data shared after taking his/her/guardian's consent.This also reflects patient centered care and online learning portfolio.This E-log book reflects my patient- centered online learning portfolio.
Under the guidance of Dr.Durga Krishna Sir[PG]
A 60 year old male farmer by occupation resident of nalgonda came to casualty with chief complaints of
Loss of appetite since 2 months
Pedal edema since 1 month
HISTORY OF PRESENT ILLNESS
The patient was apparently asymptomatic 2 years back,during this time his nephew got expired and patient started developing anxiety issues and used to take alcohol daily [previously occasional drinker] and after 15 days of expiry of his nephew patient started developing fever, sudden onset,high grade associated with generalized body pains and during this time, patient was diagnosed with hypertension.
Patient used medication for about 3 months and stopped using it.
Patient was normal upto 10 months, during this 10 months period patient started taking alcohol nearly upto 90 ml daily,and patient had sudden onset fever,high grade with low back and generalized body pains.
Then he was taken to local hospital in Miryalaguda, where he was furthre investigated and diagnosed with CKD.
Patient was on Conservative management from that time.
He was normal and used medication upto 1 year and 2 months back patient started developing loss of appetite,gradual onset associated with pedal edema,pitting type,gradual onset,grade III and not associated with any shortness of breath.
No h/o SOB,palpitations,orthopnea,dyspnea on exertion.
No h/o decreased urine output, and abdominal distention.
PAST HISTORY
H/O Hypertension since 2 years [on Tab.Nicardia 20 mg since 1 year]
H/O CKD since 1 year
Not a known case of DM,Asthma,TB,Epilepsy
PERSONAL HSTORY
Appetite - normal
Mixed diet
Bowels - Regular
Micturition - Normal
Alcohol intake occasionally upto 2 years and from then onwards daily consumes 90ml.
No other addictions
TREATMENT HISTORY
No specific treatment history
FAMILY HISTORY
His father is a known case of Hypertension
DRUG HISTORY
He has been using Tab.Nicardia 20 mg since 1 year for Hypertension.
GENERAL EXAMINATION
Patient was conscious,coherent,cooperative and examined in a well lit room
VITALS
Temperature - 98.2 F
Pulse rate - 84 bpm
Respiratory rate - 22 cpm
BP - 160/100 mmHg
SpO2 - 98% at room air
GRBS - 109 mg%
Weight - 62 kgs
PHYSICAL EXAMINATION
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing of fingers/toes - absent
Lymphadenopathy - absent
Edema of feet - present,pitting type ,below the knee from 10 days
Malnutrition - absent
dehydration - absent
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM
INSPECTION
- No parasternal heave
- JVP not elevated
- Apical impulse not visible
- No engorged veins
- Apex beat felt at 0.5 cm later to the mid clavicular line in 6th intercostal space
- Heart borders percussed
- S1 and S2 heard
- No thrills
- No murmurs
RESPIRATORY SYSTEM
- BAE +
- NVBS +
- Trachea is in central position
- No dyspnea
- No wheezing
- Scaphoid shaped abdomen
- Soft
- No tenderness
- No palpable mass
- No hernial orifices
- No free fluid
- No bruits
- Liver and spleen are not palpable
- Bowels sounds are heard
CNS
- NAD
ULTRASOUND
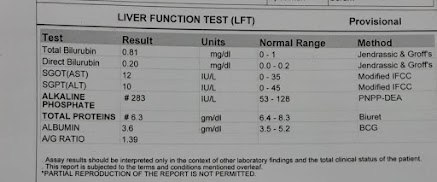
LIVER FUNCTION TEST
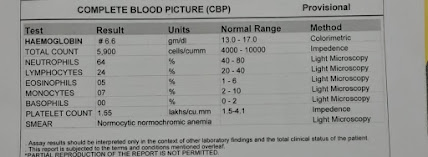
COMPLETE BLOOD PICTURE
COMPLETE URINE EXAMINATION
RANDOM BLOOD SUGAR
BLOOD UREA
SERUM CREATININE
SERUM ELECTROLYTES
SERUM CALCIUM
SERUM IRON
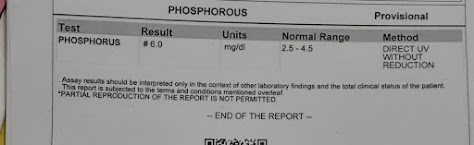
PHOSPHORUS
PROVISIONAL DIAGNOSIS
CHRONIC RENAL FAILURE
TREATMENT
Tab.Nicardia RSTARD 20 mg PO/BD
Tab Nodosis 500 mg PO/OD
Tab.Orofer XT PO/BD
Tab. Shelcal CT PO/OD
Inj. Erythropoeitin 4000IU [weekly twice]
Inj.Iron Sucrose 10MP in 50 ml NS/IU [weekly once]
Fluid restriction <1.5L/day
Salt restriction < 4 grams /day
Tab.Lasix 40 mg PO/BD
















Comments
Post a Comment